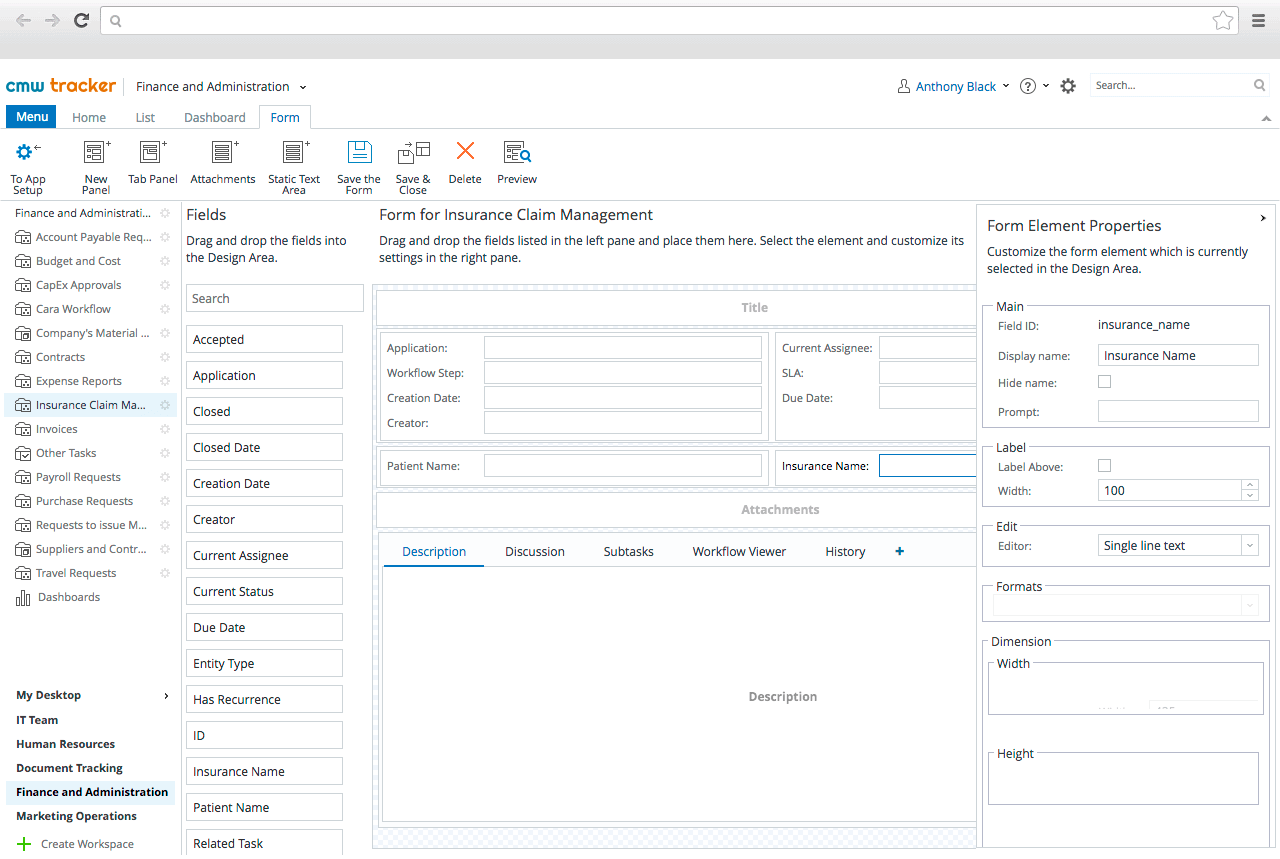
Understanding Medical Claims Processing Systems Software
In the ever-evolving landscape of healthcare, efficient management of medical claims is crucial for ensuring smooth operations and financial stability. Medical claims processing systems software has become an indispensable tool for healthcare providers, insurers, and billing agencies. This article explores the significance, functionality, and benefits of these systems, specifically focusing on insurance claims management software.
What is Medical Claims Processing Systems Software?
Medical claims processing systems software is designed to automate the processing of insurance claims. This software streamlines the entire claims lifecycle, from submission to payment. By leveraging advanced algorithms and technology, these systems reduce the administrative burden on healthcare professionals, ensuring faster processing times and improved accuracy.
Key Features of Medical Claims Processing Systems Software
1. Automated Claim Submission
One of the standout features of insurance claims management software is automated claim submission. This functionality allows healthcare providers to electronically submit claims directly to insurers, eliminating the need for paper forms. Automation reduces the risk of human error, speeds up processing times, and ensures compliance with industry regulations.
2. Real-time Claim Tracking
Medical claims processing systems provide real-time tracking of submitted claims. Providers can monitor the status of each claim, identifying issues as they arise. This transparency fosters better communication between healthcare providers and insurers, facilitating quicker resolutions to claims disputes.
3. Integrated Billing Solutions
Insurance claims management software often comes with integrated billing solutions. These systems streamline the billing process by automatically generating invoices based on the processed claims. By connecting claims data with billing, healthcare providers can reduce discrepancies and ensure accurate revenue capture.
4. Compliance and Reporting Tools
Healthcare regulations are continuously evolving, making compliance a top priority for providers. Medical claims processing systems software includes compliance tools that help organizations adhere to federal and state regulations. Furthermore, robust reporting capabilities allow healthcare organizations to analyze their claims data, helping identify trends and areas for improvement.
Benefits of Using Medical Claims Processing Systems Software
1. Increased Efficiency
By automating the claims process, medical claims processing systems significantly enhance efficiency. Healthcare providers can devote more time to patient care rather than administrative tasks. This leads to improved productivity and a more streamlined workflow.
2. Improved Accuracy
Manual claim processing is prone to errors, which can result in delayed payments or claim denials. Insurance claims management software minimizes these risks through automation, reducing the likelihood of mistakes. Enhanced accuracy ensures that providers receive timely reimbursement for services rendered.
3. Faster Reimbursement
Timely payment is vital for the financial health of healthcare organizations. Medical claims processing systems enable faster claim submissions and real-time tracking, leading to quicker reimbursement from insurers. This financial agility is essential for maintaining cash flow and ensuring operational stability.
4. Enhanced Customer Satisfaction
Efficient claims processing contributes to better patient experiences. When claims are processed smoothly and reimbursements are timely, patients are more likely to be satisfied with their overall healthcare experience. This satisfaction can enhance provider reputation and lead to increased patient retention.
Choosing the Right Medical Claims Processing System
When selecting medical claims processing systems software, healthcare providers should consider several factors:
- Scalability: The software should be able to grow with the organization, accommodating increasing claims volumes and expanding operations.
- Integration: Ensure the system can integrate seamlessly with existing healthcare IT infrastructure, including electronic health records (EHR) and practice management systems.
- User-friendly Interface: A user-friendly interface is essential for minimizing training time and ensuring staff can utilize the system effectively.
- Customer Support: Reliable customer support is crucial for resolving issues and ensuring the system operates smoothly.